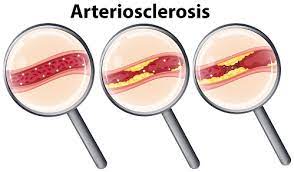
Arteriosclerosis can develop when arteries grow thick and stiff and obstruct blood inflow to organs and tissues present in the body. This gradational process, also known as hardening of the arteries, weakens arteries and can develop in various organs, utmost generally the heart. Arteries will circulate blood throughout the body, but when shrine, fat, cholesterol and other cellular waste deposits on walls of arteries arteriosclerosis can develop. Arteriosclerosis can develop into atherosclerosis. This condition can beget heart diseases, strokes, rotation problems in the arms and legs, aneurysms that can beget life threatening internal bleeding and chronic renal failure.
ARTERIOSCLEROSIS CAUSES :
Arteriosclerosis will begin in the late teens, but it usually takes decades to show signs and symptoms. Some people may experience rapidly increased arteriosclerosis during their thirties and also others may experience arteriosclerosis during their ages of fifties or sixties. Certain factors that can damage the inner area of the artery (endothelium) and can trigger the arteriosclerosis.
A number of factors can contribute to the development of arteriosclerosis:
• High blood pressure
• High cholesterol levels
• Smoking
• Blood sugar levels that are elevated
Atherosclerotic plaque is more prone to form in already-damaged arterial segments and finally burst. When the plaque breaks open, blood cell fragments called thrombocytes (or platelets) accumulate at the affected area of the
artery. These fragments can then stick together that leading to the formation of blood clots.
• High triglycerides: intake of more amount of fat in food and in the body will leads to form a triglycerides. Blood triglyceride levels are above 400 mg/dL have been linked to coronary artery disease in some people. Triglycerides, however, are not nearly as harmful as LDL(low density Lipoprotein)cholesterol.
• Diabetes: Arteriosclerosis is substantially more likely to occur in patients with poorly managed diabetes and frequent blood glucose levels that are excessive.
Genetics: Relative to other people, those who have or have had a parent or sibling with arteriosclerosis and cardiovascular disease are significantly more likely to get the condition themselves.
• Obesity: Even in the absence of other risk factors, carrying around extra weight puts a greater pressure on the heart, which in turn raises the risk of atherosclerosis owing to plaque development.
RISK FACTORS FOR ARTERIOSCLEROSIS:
Risk factors that contribute to the development of Arteriosclerosis include:
Family history: People with a family background of heart disease or arteriosclerosis are prone to higher risk for the arteriosclerosis condition.
ARTERIOSCLEROSIS SYMPTOMS:
The main symptoms of arteriosclerosis includes
• Chest pain or angina
• Leg and arm pain, and anywhere else that has a blocked artery.
• Shortness of breath.
• Fatigue
• Confusion which usually occurs if the blockage affects circulation to the brain.
•Leg muscle weakness due to poor circulation.
TYPES OF ARTERIOSCLEROSIS:
Pathologically, there are two subtypes of arteriosclerosis:
• Hyperplastic type
• Hyaline type A subdivision of arteriolosclerosis is the fibromuscular intimal thickening. There is typically hyalinosis or deposition of hyaline protein in these lesions are observed.
This includes the categories like:
• Transplants related to arteriopathy or arterial damage
• Restenosis lesions that are observed after balloon angioplasty or stenting of the coronary blood vessels of heart .
• Non-specific intimal thickening
• As age causes the temporal arteries, which are located around the forehead and temples, to enlarge. Intimal expansion without atherosclerotic alterations in the walls characterises transplant arteriopathy. Both major and small muscle arteries and veins are impacted by transplant arteriopathy.It commonly causes inflammation in one layer or more than 3 layers in the blood vessel walls. Generally, the intima layer is affected more than the media or adventitia layers, but all three layers may also be affected. After inflammation there is fibrosis and finally calcification and thrombosis may occur.
ARTERIOSCLEROSIS DIAGNOSIS:
• Blood tests: Blood tests can help to detect increased levels of cholesterol and blood sugar levels in blood that may increase the risk of arteriosclerosis.
• Doppler ultrasound: It is a special ultrasound device (Doppler ultrasound) which is used to measure the blood pressure at various points along leg or arm. These measurements can help doctor to measure the degree of any artery blockages, as well as the speed of blood flow in the arteries.
• (ECG)Electrocardiography: An electrocardiogram which measures the electrical activity of the heart. This test can measure the proper functioning of the heart and can often detect the presence of heart disease.
• Stress test: stress test, also known as exercise stress test. It is employed to compile data on how effectively the heart performs throughout any physical activity. An exercise stress test might identify cardiac issues that might not otherwise be apparent since physical activity causes the heart to beat faster and harder than it does during the majority of regular activities. During this stress test, the patient often exercises on a treadmill or stationary cycle while having their heart rate, blood pressure, and breathing rate checked.
• Ultrasound: An ultrasound scanner creates an image of the interior of the body using sound waves. This will make it easier to assess blood pressure throughout the body. Any changes in blood pressure might indicate where an artery blockage is located. Research can also be done using ultrasound examinations.
COMPLICATIONS OF ARTERIOSCLEROSIS:
If arteriosclerosis is not diagnosed and treated properly then it leads to serious complications like:
• Carotid artery disease: These arteries provide blood circulation to the brain. When the blood supply is limited, patients can suffer from strokes or Ischemic attacks.
• Coronary artery disease: These arteries will provide blood circulation to the heart, when the blood supply to the heart is limited, it can cause angina pectoris and heart attack.
• Heart attack: If one of the plaques in the coronary arteries ruptures, causing blood clots to develop. A heart attack will result if a blood clot restricts the flow or supply of blood to the heart.
• Aneurysm: If arteriosclerosis weakens the blood vessel walls, it may result in the development of an aneurysm, which is a blood vessel bulge. If the aneurysm grows too much, then the condition is more severe,there is a danger. Blood vessels will rupture, which can cause potentially fatal internal bleeding and also cause organ damage.
• Chronic renal failure: These supply blood to the kidneys; if the blood supply becomes limited, there is serious risk of a developing chronic renal failure.
• Peripheral arterial disease: The arteries to the limbs, usually the legs, are blocked.
ARTERIOSCLEROSIS TREATMENT:
Treatment used for arteriosclerosis includes a healthy diet, adequate exercise and medication to control or possibly reverse condition. Medications used to treat arteriosclerosis are mainly depends upon the location of enlarged blood vessels and other underlying conditions may include.
• Cholesterol medications can helps to protect heart arteries.
• Aspirin will prevent platelets from forming blood clots.
• B-blocker drugs help lessen chest discomfort, the risk of a heart attack, and abnormal heart rhythm in addition to lowering blood pressure and heart rate.
• Angiotensin-converting enzyme (ACE) inhibitors can help to reduce the blood pressure and lower the possibility of development of heart attack.
• Calcium channel blockers and diuretics misc (water pills) can reduce blood pressure.
• A clot-busting drug may dissolve blood clots