INFLAMMATORY BOWEL DISEASE (IBD):
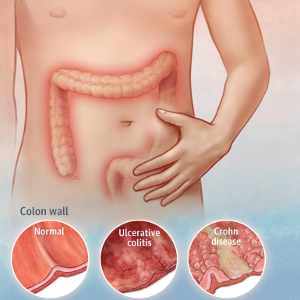
Inflammatory bowel disease( IBD) is an idiopathic complaint caused by a deregulated vulnerable response to host intestinal microflora. The term IBD is generally used to two bow complaint having multitudinous parallels but the conditions generally have distinctive morphological appearance. These two conditions are ulcerative colitis and Crohn’s complaint
• Ulcerative colitis: This condition causes long- lasting inflammation and blisters(
ulcers) in the inmost filling of the large intestine( colon) and rectum. Ulcerative colitis often begins in the rectum and progresses above into the sigmoid colon, descending colon, transverse colon, and rarely the whole colon. The colonic contents may infrequently back flow in the terminal ileum in durability, causing’ back wash ileitis’ in about 10 of cases.
• Crohn’s disease: Crohn’s complaint may involve any portion of the gastrointestinal tract but affect most generally 15- 25 cm of the terminal ileum which may extendinto the caecum and occasionally into the thrusting colon. Both ulcerative colitis and Crohn’s disease generally involve severe diarrhoea, abdominal pain, and fatigue and weight loss.
CAUSES OF INFLAMMATORY BOWEL DISEASE:
1. Immunological factors
The precise aetiology of IBD is unknown, however it is the result of a malfunctioning susceptible system. A duly performing vulnerable system attacks foreign organisms, similar as contagions and bacteria, to cover the body. In IBD, the vulnerable system(immune) responds inaptly to environmental triggers, which leads to cause gastrointestinal tract inflammation.
2. Inheritable factors
There’s about 3 to 20 time advanced frequency of circumstance of IBD in first
degree cousins. This is due to inheritable disfigurement causing diminished epithelia hedge function. There’s roughly 50 chance of development of IBD( Crohn’s complaint about 60, ulcerative colitis about 6) in monozygotic halves. Still there’s no clear link between the abnormal genes and IBD.
Exogenous factors:
i) Microbial factors: Microbial factors (bacteria, viruses, protozoa, and fungus) have been suspected but there has been no conclusive proof.
ii) Psychosocial factors: Those who are too sensitive, reliant on others, and unable to express themselves, as well as big life events such as illness or death in the family, divorce, interpersonal disputes, and so on, have irritable colon or have symptoms exacerbated.
iii) Smoking: Role of smoking in causation of Crohn’s disease has been reported.
iv)Oral contraceptives: An increased risk to develop Crohn’s disease with long
term use of oral contraceptive has been found in some studies but there is no
such increased risk of ulcerative colitis.
SYMPTOMS OF INFLAMMATORY BOWEL DISEASE:
Inflammatory bowel disease symptoms vary, depending on the inflexibility of
inflammation and where it Occurs. Symptoms may range from mild to severe. Signs and symptoms that are common to both Crohn’s complaint and ulcerative colitis include Diarrhoea, fever and fatigue, abdominal pain and cramping, blood in coprolite, reduced appetite, unintended weight loss. Other symptoms may include Constipation, blisters or swelling in the eyes, draining of pus, mucus, or droppings from, around the rectum or anus( fistula), common pain and lump, mouth ulcers, rectal bleeding and bloody droppings, blown epoxies, tender, red bumps( nodes) under the, skin which may turn into skin ulcers.
DIAGNOSIS OF INFLAMMATORY BOWEL:
ETO Crohn’s disease is diagnosed through a medical history, physical exam, imaging tests to look at the intestines, and lab tests.
• General investigation: Physical Examinations include, checking for signs such as paleness (caused by anemia) or tenderness in the abdomen, skin rash, swollen joints, or mouth ulcers and tenderness in stomach (caused by inflammation) and recording of patient’s history.
• Blood tests: To look for changes in Red blood cells: When red blood cells are fewer or smaller than normal, a patient may have anemia.
• White blood cells: When a person’s white blood cell count is greater than usual, he or she may be suffering from inflammation or infection anywhere in the body. Blood tests are also helpful to find antibodies. The presence of certain antibodies can sometimes help diagnose types of inflammatory bowel disease i.e. Crohn’s disease or ulcerative colitis.
• Stool tests: A stool test is helps to analysis of a sample of stool, to rule out other
causes of GI diseases.
• Upper gastrointestinal (UGI) series: It examines the upper part of the digestive
tract.
• Upper gastrointestinal endoscopy: looks at the interior lining of oesophagus ,
stomach and duodenum Colonoscopy or flexible sigmoido- scopy: Colonoscopy is
often is usually preferred test because to examine the entire colon. Sigmoidoscopy is reaches only the lowest part of the colon.
• Abdominal IX-ray: This test can show possible obstructions in the tummy. Barium enema This test looks at the Large intestine( colon).
• Reckoned tomography( CT): check-up Motorized tomography reviews use a
combination of X-rays and computer technology to produce images. CT reviews can diagnose both Crohn’s complaint and the complications seen with the complaint.
• Glamorous resonance imaging( MRI): MRI uses a glamorous field and beats of radio surge energy to give film land of organs and structures inside the body. The pathologic realities of a fistula, a sinus tract, and an abscess can be detected in the static anorectal region by using MRI.
• Barium enema:This particular test uses an X-ray to examine the whole large intestine. An enema is used to deliver barium, a discrepancy result, into the intestine. Air is occasionally introduced as well. The barium fleeces the filling, forming rectum, colon, and small intestine characteristics. This test is infrequently used presently, and it can be dangerous because the pressure needed to inflate and cover the colon can lead to rupture of the colon. For people with severe symptoms, flexible sigmoidoscopy combined with a CT check-up is a better volition
INFLAMMATORY BOWEL DISEASE TREATMENT:
Treatment for IBD depends on the soberness of the complaint. Utmost people are
treated with drug. Some people whose symptoms are touched off by certain foods are suitable to control the symptoms by avoiding foods that upset their bowel. Like largely seasoned foods or dairy products. Each person may witness ulcerative colitis else, so treatment is acclimated for each existent. Emotional and cerebral support is also important. The main points of treatment are to
• Reduce symptoms, known as converting absolution( a period without symptoms),
• Maintain absolution.
Anti-inflammatory medicines:
Anti-inflammatory medicines are frequently the first step in the treatment of seditious bowel complaint. They include
i) Amino salicylates( ASAs): similar as Sulfasalazine, Mesalamine, Balsalazide
and Olsalazine are specifics that help to reduce inflammation and effective
in ulcerative colitis.
ii) Corticosteroids: These medicines, which include prednisone and
hydrocortisone are a more important type of specifics used to reduce
inflammation. They can be used with or rather of ASAS to treat a flare- up
if ASAS alone aren’t effective.
iii) Immunosuppressant’s: Immunosuppressant’s similar as Azathioprine, 6-
mercaptopurine, methot- rexate, cyclosporine are frequently used and can
make a pronounced enhancement at a low cure with many side goods.
Other medicines may be given to relax the case or to relieve pain,
diarrhoea, or infection. Sometimes, symptoms are severe enough that the
person must be rehabilitated.
Other Medications:
Certain ulcerative colitis symptoms necessitate the use of additional drugs.
(i)Antibiotics: Patients with ulcerative colitis who develop fevers will almost certainly be given antibiotics to assist prevent or manage infection.(e.g., Metronidazole, Ciprofloxacin, Rifaximin etc)
(ii) Antidiarrhoeal medications: For severe diarrhoea, loperamide may be effective. Nevertheless, antidiarrheal drugs should be used with extreme caution since they may raise the risk of toxic megacolon.
(iii) Iron supplements: In chronic intestinal bleeding, person may develop iron deficiency anemia and be given iron supplements.
(iv) Bowel rest: Sometimes Crohn’s disease symptoms are severe and a person may need to rest bowel for a few days to several weeks.Bowel rest entails simply drinking clear liquids or not eating anything. Nutritions are provided to the patient intravenosly through a special catheter, or tube, inserted into a vein in the patient’s arm.
(v) Surgery: Even with medication treatments, up to 20% of people will need surgery to treat their Crohn’s disease. Although surgery will not cure Crohn’s disease, it can treat complications and improve symptoms.