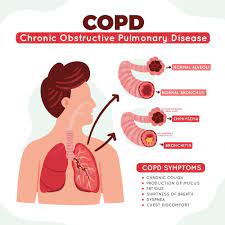
CHRONIC OBSTRUCTIVE PULMONARY DISEASE(COPD)
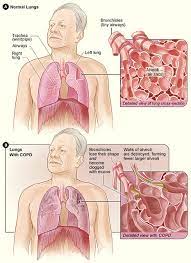
It is also called COAD(chronic obstructive airway disease. COPD/COAD is a group of clinicopathological conditions characterized by airway limitation due to chronic/partial/complete obstruction to the airway at any level from the trachea to the smallest airways that is not fully reversible. COPD is a progressive disease with Emphysema and chronic bronchitis.
CHRONIC BRONCHITIS:
- It is a common condition where persistent cough with expectoration on most days for at least 3 months of the year for 2 or more consecutive years, the cough is caused by over-secretion of mucus.
- When smoking/irritants/chemicals enter the lungs it increases the size and
number of the bronchial mucinous glands and goblet glands(these are the glands
that are responsible for the production of mucus) resulting in an increase in mucus production causing airway obstruction. This results in a decreased amount of oxygen in the lungs and an increased amount of carbon dioxide leads to hypercapnia which turns the body into blue color hence called blue bloaters.
EMPHYSEMA:
- Emphysema is nothing but a cause of the structural abnormality.
- These are called pink puffers
- It’s a long-term progressive irreversible disease of the lungs that affects the respiratory unit leading to damage to the wall which results in loss of elasticity leads to permanent enlargement of air sacs and ultimately causes air trapping.
- Emphysema is a chest condition that falls under the umbrella term of COPD.
- Emphysema causes shortness of breath and in people with emphysema, the air sacs in the lungs are damaged.
COPD SYMPTOMS:
Symptoms of COPD include,
• Persistent productive cough
• Wheezing
• Excess of phlegm Or sputum
• Shortness of breath
• Trouble while taking a deep breath
• Lack of energy (tiredness)
• Loss of weight
• Swelling of ankles, feet, Or legs
• Chest tightness
• Recurrent respiratory infections
• Chest pain
• Coughing up blood
• Obesity
• Cyanosis(blue colour on skin, lips or in fingernails)
COPD STAGES
The four different stages of COPD include,
Stage 1: Mild COPD (early stage)
At this stage, the people may experience symptoms like shortness of breath and productive cough. The amount of airflow in this stage is about 80% of normal.
Stage 2: Moderate COPD
At this stage, the symptoms get worsen from stage 1 coughing, and mucus production may become severe, wheezing and people may experience shortness of breath during physical activity. The amount of airflow in this stage is between 50%-79% of normal.
Stage 3: Severe COPD
This stage is considered a severe stage where people experience severe symptoms like chest tightness, wheezing, swelling in ankles, and trouble in deep breathing. The amount of airflow in this stage is between 30%-50% of normal.
Stage 4: very severe COPD (chronic)
The oxygen level in the blood becomes low, which increases the risk of developing heart Or lung failure. Flare-ups and normal exacerbation can be life-threatening. The amount of airflow is less than 30% of normal.
CAUSES OF COPD:
The main causes of COPD include,
1. Cigarette smoking
• Smoking is the main cause of COPD and is thought to be responsible for about
90% of cases
• The harmful chemicals which are present in the smoke can damage the lining of the lungs and the airways.
2. Fumes and dust
The fumes and dust which increase the risk of COPD include
• Welding fumes
• Cadmium dust
• Silica dust
• Coal dust
3. Hair spray
4. House paint
5. Air pollution
• Exposure to pollution over a long period of time can affect the proper working of
lungs and may increase the risk of COPD.
6. Alpha 1 antitrypsin deficiency(AAt)
• About 1% of people are suffering from COPD. It is a genetic disorder that lowers the level of a protein called alpha-1 antitrypsin (AAt). It is a type of protein secreted in the liver and released into the bloodstream to protect the lungs.
• The alpha 1 antitrypsin deficiency may cause lung disease or liver disease or
sometimes it is responsible for causing both types of disease.
• This disorder can be treated by replacing that particular protein which further
prevents damage to the lungs.
RISK FACTORS OF COPD:
• Smoking or secondhand smoke
• History of respiratory infections
• People with asthma are more prone to the development of COPD
• Exposure to chemicals and dust
• Lung irritants like fumes
• Exposure to air pollution
• Genetic abnormalities
• Biomass fuel exposure
• Abnormal lung development
• Accelerated aging
COMPLICATIONS OF COPD:
COPD can cause many serious complications including,
1. Lung cancer: People with COPD have more risk of developing lung cancer.
2. Heart problems: Due to decreasing the level of oxygenated blood, may cause the risk of heart diseases including heart attack, and arrhythmias (irregular heartbeats).
3. Respiratory infections: People with COPD are more prone to catch colds, flu, and pneumonia, Any respiratory infection worsens the conditions, makes it much more difficult to breathe, and causes damage to the lung tissues.
4. Anxiety disorders
5. Depression: COPD can contribute to the development of depression due to difficulty in breathing can keep you from doing all the physical activities that you enjoy.
6. Pneumothorax: it is a condition where the lungs are gets collapsed. It occurs when the air enters the space in between the lungs and the chest wall.
7. Skeletal muscle dysfunction: The muscle strength, endurance, and muscle
Capillarity will decrease in people with COPD.
8. Acute respiratory failure: It happens suddenly when the lungs cannot release
the required amount of oxygen into the blood. Respiratory infections and pneumonia
can cause fluid buildup in the lungs.
9. Pulmonary hypertension: An increase in blood pressure affects the arteries in the lungs and in the heart. It usually worsens during exercise, sleep, and exacerbation.
10. Severe weight loss and malnutrition
PREVENTION OF COPD:
• Cessation of smoking
• Avoid passive smoking
• Breathing exercises
• Breathing in warm moist air
• Mild physical activity can strengthen muscles
• Eat healthily, get the nutrition your body needs
• Ensure your are vaccinated(influenza vaccine, pneumococcal vaccine)
DIAGNOSIS OF COPD:
1. Medical history:
To diagnose people with COPD the physician will ask questions like,
• Do you have a history of respiratory infections?
• Do you smoke?
• Do you cough up sputum?
• Do you have any trouble while taking a deep breath?
• Do other members of your family have COPD?
• What is the pattern of symptom development?
• Any history of exacerbation?
2. Physical examination:
• Listening to lungs and heart
• Checking of blood pressure
• Examining the nose and throat
• Checking the swelling of the ankles and feet
3. Tests to diagnose COPD:
• Pulmonary (lung function test): Uses a test called spirometry to check the
function of the lungs. This test measures the amount of air during the inhale and
exhale and checks whether the lungs deliver enough oxygen into the blood.
Other test includes,
• Pulse oximetry: This will measure the amount of oxygen in the blood.
• ECG(electrocardiogram ): helps to check the functions of the heart.
• Chest X-ray: This test can identify emphysema and also other lung
problems and heart problems.
• CT scan: This scan helps to detect emphysema. It is also used to screen for
lung cancer.
• Arterial blood gas analysis: this is a blood test that measures how well the
lungs are carrying oxygen into the blood and removing carbon dioxide from
the blood.
• Alpha 1 Antitrypsin deficiency screening: This screening test is performed for
patients under the age of 45 or for those people with strong family history.
COPD TREATMENT:
MEDICATION:
1. Bronchodilators:
• Bronchodilators relieve bronchospasm and prevent airway obstruction by
increasing oxygen distribution throughout the lungs.
• This medication is delivered through a metered dose inhaler (MDI) by nebulization or by pill or liquid dosage form.
2. Corticosteroids:
• Use both inhalational and systemic corticosteroids for the treatment of COPD.
• A short course of oral glucocorticoid benefits some patients with COPD.
• Prevent acute exacerbation of COPD.
• But inhaled corticosteroids are beneficial in advanced COPD with frequent
exacerbation they should not be used in mild or moderate cases.
3. Antibiotics/ antivirals:
• In COPD mucus production is more which makes patients more prone to lung
infections, which can further damage wreaked lungs Patients may need to take
antibiotics to stop bacterial infections.
4. Mucolytics:
• These are the agents which can liquefy the mucus plugs in the airways so the patient can cough it out more easily.
5. Vaccinations:
• COPD makes patients more prone to lung infections.
• Respiratory infections are more dangerous during COPD
• It s important to get vaccine shots, influenza vaccine, pneumococcal vaccine,
and tetanus booster to prevent this infection
CLick Here To Buy
OXYGEN THERAPY:
• If the oxygen saturation of patients is low, oxygen therapy is required
• In mild to moderate cases oxygen can be given in a hospital setting and stopped once the patient is stable
• Long-term oxygen therapy treatment (LTOT) should be used at least 16 hours/per day
• Oxygen can be taken through Nasal tubes or a mask
• The tubes from machines are so long that, patients will be able to move around the home while connected portable oxygen tanks are also available.
• Do not smoke while on oxygen increased level of oxygen is highly flammable, a lit
cigarette could cause a fire or explosion.
SURGERY:
Surgery is usually only suitable for the small number of people with severe increased COPD whose symptoms are not controlled by medicine.
• Bullectomy: Large air sacs formed in the lungs when the walls of alveoli are destroyed are known as bullae. During bullectomy bullies are removed which makes breathing more comfortable.
• Lung volume reduction surgery: An operation to remove badly damaged sections of the lung to allow the healthier parts to work better and make breathing more comfortable.
• Lung transplant: An operation to remove and replace a damaged lung with a healthy lung from a donor.