ALCOHOLIC LIVER DISEASE
Alcoholic Liver disease is a pattern of progressive seditious liver injury that is associated with a long-term heavy intake of alcohol. The pathogenesis of this disease isn’t fully understood. Though alcoholic liver disease is most likely to do in people who drink heavily numerous times, the relationship between drinking and alcoholic liver disease is very complex. Not all heavy alkies develop alcoholic liver disease, and the complaint can do in people who drink only relatively.
Cases who are oppressively affected present with subacute onset of fever, hepatomegaly leucocytosis, pronounced impairment of liver function(e.g. of this include hostility, coagulopathy), and instantiations of portal hypertension(e.g., ascites, hepatic encephalopathy, variceal hemorrhage). Still, milder forms of alcoholic liver complaint frequently don’t beget any Symptoms.
The alcoholic liver complaint generally persists and progresses to cirrhosis if heavy alcohol use continues. However, alcoholic liver complaint resolves sluggishly over weeks to months, occasionally without endless squeal but frequently with residual cirrhosis, If alcohol use ceases. Of all habitual heavy drinkers, only 15- 20 develop hepatitis or cirrhosis, which can do concomitantly or in race.
EPIDEMIOLOGY
Alcohol abuse is the most common cause of serious liver complaints in Western societies. The true frequency of alcoholic liver disease, especially of its milder forms, is unknown because cases may be asymptomatic and now seek medical attention.
ALCOHOLIC LIVER DISEASE CAUSES
Alcoholic liver disease usually occurs when the liver is damaged by the inordinate consumption of alcohol. How alcohol damages the liver and why it does so only in a nonage of heavy alkies isn’t clear. It’s known that the process of breaking down ethanol; the alcohol in beer, wine, and liquor produces largely poisonous chemicals, similar to acetaldehyde. These chemicals spark inflammation that destroys liver cells. Over time, webs- such as scars and small knots of tissue replace healthy liver towels, snooping with the liver’s capability to serve. This unrecoverable scarring, called cirrhosis, is the final stage of alcoholic liver disease.
Heavy alcohol use can lead to severe liver disease, and the threat increases with the length of time and quantum of alcohol drunk. But because numerous people who drink heavily or binge drink now develop alcoholic liver complaints or cirrhosis, it’s likely that factors other than alcohol play a part. These include:
• Other types of hepatitis: Long-term alcohol abuse worsens the liver damage caused by other types of hepatitis, especially hepatitis C.
• Malnutrition: Numerous people who drink heavily are glutted, either because they eat inadequately or because alcohol and its Poisonous by-products help the body from duly absorbing and breaking down nutrients, especially protein, certain vitamins, and fats. In both of these cases, the lack of nutrients contributes to liver cell damage.
• Sex: Women have an advanced threat of developing alcoholic liver complaints more than men do. This difference may affect differences in the way alcohol is reused by women.
• Inheritable factors: A number of inheritable mutations have been linked that affect the way alcohol is broken down in the body. Having one or further of these mutations may increase the threat of alcoholic liver disease.
• Other factors which may increase threat include
Type of beverage( beer or spirits are unsafe than wine) Binge drinking Obesity Alcohol and obesity may- have a synergistic effect on the liver, that is, their concerted effect is worse than the effect of either of them alone.
SYMPTOMS OF ALCOHOLIC LIVER DISEASE
It may not have symptoms in the early stages. Symptoms may lead to worse after a period of heavy drinking.
Digestive symptoms include:
• Pain and swelling in the tummy and tenderheartedness
• Dropped appetite and weight loss
• Nausea and vomiting
• Fatigue
• Sot mouth and increased thirst Bleeding from enlarged modes in the walls of the lower part of the esophagus. Skin problems include:
• Similar to the unheroic colour(yellow) in the skin, mucus membranes, or eyes(jaundice).
• Small, red spider- suchlike modes on the skin.
• Veritably dark or pale skin.
• Greenishness on the bases or hands.
• Itching Just about everyone who has an alcoholic liver complaint is glutted. Drinking large quantities of alcohol suppress the appetite, and heavy alkies get the utmost of their calories in the form of alcohol.
COMPLICATIONS
Complications of alcoholic liver complaints include:
• Increased blood pressure in the portal vein: Blood from the intestine, spleen, and pancreas enter the liver through the portal vein. However, this blood backs up, leading to increased pressure within the tone( portal hypertension), If scar tissue slows normal rotation through the liver.
• Enlarged modes: When( varies) V rotation through the portal tone is blocked, blood may back up into other blood vessels in the stomach and esophagus. Massive bleeding in the upper stomach or esophagus from these blood vessels is a life-changing exigency that requires immediate medical care.
• Jaundice: It occurs when the liver isn’t suitable to remove bilirubin; the residue of old red blood cells from the blood. Bilirubin builds up and is deposited in the skin and the whites of the eyes, causing an unheroic(yellow) color.
• Hepatic encephalopathy: A liver damaged by alcoholic liver complaint has trouble removing poisons from the body typically one of the liver’s crucial tasks. The buildup of poisons can damage the brain, leading to changes in internal state, geste, and personality( hepatic encephalopathy). Signs and symptoms of hepatic encephalopathy include obliviousness, confusion, mood changes, and in the
most severe cases coma.
ALCOHOLIC LIVER DISEASE DIAGNOSIS
Common considerations in alcoholic cases with hostility include habitual pancreatitis with biliary strictures and pancreatic biliary tumors. Changes in the internal status of issues with alcoholic liver complaints don’t always indicate the air presence of hepatic encephalopathy. Realities(e.g. subdural be barred by hematomas) should be attained by a reckoned tomography( CT) check-up of the brain.
1. CBC Count: A complete blood cell( CBC) count generally reveals some degree of neutrophilic leucocytosis with a pandemic. Generally, this is moderate; still, infrequently, it’s severe enough to give a leukemoid picture. Alcohol is a direct gist suppressant, and moderate anemia may be observed. In addition, alcohol use characteristically produces a moderate increase in mean corpuscular volume. Thrombocytosis may be observed as part of the seditious response; again, myelosuppression or portal hypertension with splenic insulation may produce
thrombocytopenia.
2. Screening Blood Tests: Screening blood tests to count other conditions( applicable in any case with alcoholic liver disease) may include the following:
• Hepatitis B face antigen( HBsAg) detects hepatitisB.
• Anti-hepatitis C contagion by enzyme-linked immunosorbent assay( ELISA) detects hepatitis C.
• Ferritin and transferrin achromatism descry hemochromatosis.
• Jaundice with fever can be caused by gallstones producing cholangitis and is suggested by a disproportionate elevation of the alkaline phosphatase( ALP) position.
3. Liver Function Tests: Liver enzyme situations parade a characteristic pattern. In utmost cases, the aspartate aminotransferase( AST) position is relatively elevated, whereas the alanine aminotransferase( ALT) position is in the reference range or only mildly elevated. This is the contrary of observed in utmost other liver conditions.
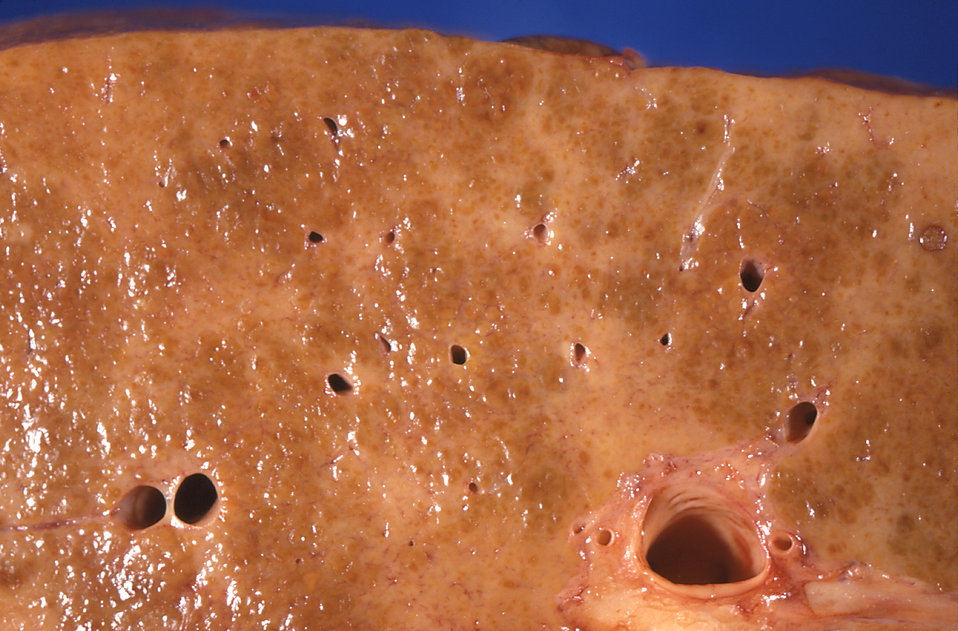
4. Ultrasonography: Ultrasonography is the favored imaging study in assessing cases with suspected alcoholic liver complaints. This modality provides a good evaluation of the liver and other viscera, and it permits guided liver biopsy.
5. Liver biopsy: Liver vivisection isn’t always needed in the evaluation of alcoholic liver complaints, but it may be useful in establishing the opinion, in determining the presence or absence of cirrhosis, and in banning other causes of liver disease.
ALCOHOLIC LIVER DISEASE TREATMENT
In utmost cases with alcoholic liver complaints, the illness is mild. Their short-term prognostic is good, and no specific treatment is needed. Hospitalization isn’t always necessary. Alcohol use must be stopped, and care should be taken to insure good nutrition; furnishing supplemental vitamins and minerals, including folate and thiamine, is reasonable. Cases that are coagulopathic should admit vitamin K parenterally.
Anticipate symptoms of alcohol pullout, and manage them meetly. Cases with severe alcoholic liver disease may profit over the short term from specific curatives directed toward reducing liver injury, enhancing hepatic rejuvenescence, and suppressing inflammation. For the long term, pretensions include enhancement of liver function, forestalment of progression to cirrhosis, and reduction of mortality.
• Cessation of Alcohol Intake: Cessation of alcohol use is the dependence on treatment of alcoholic liver disease.
• Liver Transplantation: Orthotropic liver transplantation is extensively used in cases with end-stage liver complaints. Utmost cases with active alcoholic liver complaints are barred from transplantation because of ongoing alcohol abuse. In utmost liver transplantation programs, cases must hesitate from alcohol for at least 6 months before they can be transplantation, and considered for a thorough psychosocial evaluation must demonstrate that cases have a low liability of returning to alcohol abuse.
• Surgical Considerations: Cases with an acute alcoholic liver complaint are at high threat of developing hepatic failure following general anesthesia and major surgery. Because postoperative mortality rates are high, surgery should be avoided in the setting of acute alcoholic liver disease unless it’s indispensable. If patients remain abstinent, the alcoholic liver disease generally resolves over time, permitting surgery to be accepted with a mainly reduced threat.
• Herbal Agents Milk thistle: Herbal agents have also been tried in alcoholic liver complaints. Silymarin is the active component in milk thistle and is a member of the flavonoids. The precise medium of its hepatoprotective agreement isn’t known, but it’s presumably related to its antioxidant parcels. In humans with mild alcoholic liver complaints, silymarin improves liver chemistry test results. Milk thistle is generally safe, but can beget diarrhea and nausea.
